So what is the definition of health system? what is concerned in a health system? Who are playing a role in this system?
The health system consists of ministry of health, health providers, health services organizations, pharmaceutical companies, health financing bodies, etc. Roemer (1991) defined a health system as "the combination of resources, organization, financing and management that culminate in the delivery of health services to the population." The World Health Organization (2000) redefined the main purpose in its definition of a health system as "all activities whose primary purpose is to promote, restore, and maintain health." In recent years, the definition of "purpose" has been further extended to include the prevention of household poverty due to illness.
As you know, the health systems comprises both private and public health services. In the public sector, there are many parts in a health system. Each part operates at different level, serving different scope of communities.Smaller systems maybe self contained and limited scale and scope, such as those involved in running a clinic or managing a health information system. Larger systems might involve the coming together of various smaller systems. For instance, the hospitals provide coherence at community or national level. In the district hospitals, there maybe limited equipments and workforce. So, they would refer the patients to the provincial hospital if they are not capable to manage the case due to the setback. For example, after the 1st eruption of Gunung Merapi on 26th of october, those patients with burnt injury below 40% were sent to the nearest hospitals, whereas those with burnt injury more than 40% were directly sent to RS Sardjito.
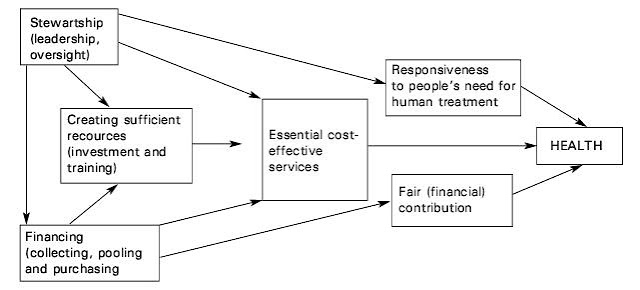
In health system, each object (MOH, health financing bodies, health providers, health services organizations, pharmaceutical companies, communities, etc) interconnect each other, serving for few functions:
1) oversight/stewardship and leadership (policymaking, regulation): This is usally the responsibility of government. It sets the context and policy framework. For those who are playing a role in this part, they may question: what is the institutional framework in which the system and its many actors should function? which activities should be coordinated and how? what are the trends in health priorities and resource generation and their implications for the next 10,20, or 30 years? what information is needed and by whom to ensure effective decision making on health matters, including prevention and mitigation of epidemics? An additional central function is generating appropriate data for policymaking. These range from public health surveillance data to health system performance and provide the basis for accessing health status, regulating the sector and tracking health system perforrmance, effectiveness and impact. reading until here, u may ask: How to access health status? Health status can be measured by measuring the morbidity and mortality rates (eg. maternal mortality rate, infant mortality rate), life expectancy,etc. Therefore, a good stewardship and leadership will:
- ensure that health authorities take responsibility for steering the entire health sector and dealing with future challenges as well as with the current problems.
- Set direction by defining national health policies, strategy and plan, so that high policy goals will be achieved (such as health equity, people centeredness, sound public health policy, effective and accountable governance). By such, the goals can be translated into its implication for financing, human resources, pharmaceuticals, technology, infrastructure and service delivery (including cost-effective services).
- have an effective regulation, backed up by legal measures and enforcement mechanisms
- effective policy dialogue with other sectors
- networks of close-to-client primary care, organized as health districts or local area networks, with the back up of specialized and hospital services, responsible for defined populations.
- provision of benefits with comprehensive and integrated interventions, that respond to full range of health problems of their populations
- standards, norms and guidance to ensure access and essential dimensions of quality (safety, effectiveness, integration. continuity, people centeredness)
- mechanisms to hold providers accountable for access and quality and to ensure consumer voice.
4) managing resources: In the previous post, i have described the input of fish pond system by using 5M. Similarly, 5M (man, money, materials, method, machine) is applied in health system to describe the input/resources.
- Man? This implies the human resources. How to manage the human resources? By: 1) arrangement to achieve sufficient of right mix (numbers, diversity, and competencies); 2) payment systems to provide the right kind of incentives; 3) regulatory mechanisms to ensure system wide deployment and distribution in accordance with needs; 4) establishment of job related norms, deployment of support systems and enabling work environments; 5) meachanisms to ensure cooperation of all stakeholders (health worker advisory groups, donor coordination groups, private sector, professional associations, communities, client/consumer groups)
- Money? as what i have discussed before this.
- Materials? "Materials" refer to medical products and information. 1) Medical products should be regulated for marketing authorization and safety monitoring, by setting relevant legislation and enforcement mechanisms. Besides that, there should be national lists of essential medical products, national diagnostic and treatment protocols, and standardized equipment per levels of care, to guide procurement, reimbursement and training. A supply and distribution system is established to ensure universal access to essential medical products. Also, a national medical products availability and price monitoring system are established as well as the national programme on promoting rational prescribing. 2) Health information on a) the progress in meeting health challenges and social objectives (by doing household surveys, epidemiology surveillance); b) health finance (by doing financial analysis); c)pharmarceuticals; d) appropriateness and cost of technology; e) distribution and adequacy of infrastructure; f) access to care and on the quality of services provided.
- Method? it implies the method of regulating the whole system (how to regulate the system, how to manage the finance, how to access health status, how to improve the quality of service, how to access the quality of health service, etc). They are managed by the legislation and policies.
- Machine? It refers to the technology, the equipment used for telecommunicating, diagnosis, treatment, etc. Health information about the appropriateness and cost of technology are obtained and then further analyzed. Besides that, a system is created to ensure universal access to essential health technologies.
What factors influence the health system?
This figure would take different shapes in different societies, but everywhere individuals form part of a network of family and community members who are concerned about their health. This network prescribes or advises how to prevent illness and what to do in case of ill health. In many societies, mothers and grand mothers are key figures in early childcare. They determine nutritional and hygiene practices, alert children to dangers, provide care in case of disease, and teach children the basics of self-care.
At the other end of the spectrum, a public authority is responsible for the well being of all people inhabiting its territory. Nowadays governments of states organise public health care and, to some extent, regulate private health care initiatives. Through other social services (e.g., education, social welfare), through laws and taxes and police and army, governments are supposed to assure their citizens the resources to survive and live in peace. Since time immemorial this has been the duty of rulers, although each society has developed its own ways of ensuring ‘health for all’.
Reference:
1) http://siteresources.worldbank.org/HEALTHNUTRITIONANDPOPULATION/Resources/281627-1154048816360/AnnexLHNPStrategyWhatisaHealthSystemApril242007.pdf
2) WHO 2010. Key Components of A Well Functioning Health System.
3) Corlien M. Varkevisser, Indra Pathmanathan, Ann Brownlee; Designing And Conducting Health System Research Projects, Volume 1: Proposal Development and Fieldwork; KIT Publishers and the International Development Research Centre (IDRC), in association with the Africa Regional Office (AFRO) of the World Health Organization; 2003.
4) http://regional.kompas.com/read/2010/10/26/20523040/RS.Sardjito.Terima.Korban.Luka.Bakar
5) Prof. Dr. Laksono; Lecture Block 4.2: Introduction of Block 4.2 And Health System And Its Outcome.
Reference:
1) http://siteresources.worldbank.org/HEALTHNUTRITIONANDPOPULATION/Resources/281627-1154048816360/AnnexLHNPStrategyWhatisaHealthSystemApril242007.pdf
2) WHO 2010. Key Components of A Well Functioning Health System.
3) Corlien M. Varkevisser, Indra Pathmanathan, Ann Brownlee; Designing And Conducting Health System Research Projects, Volume 1: Proposal Development and Fieldwork; KIT Publishers and the International Development Research Centre (IDRC), in association with the Africa Regional Office (AFRO) of the World Health Organization; 2003.
4) http://regional.kompas.com/read/2010/10/26/20523040/RS.Sardjito.Terima.Korban.Luka.Bakar
5) Prof. Dr. Laksono; Lecture Block 4.2: Introduction of Block 4.2 And Health System And Its Outcome.


No comments:
Post a Comment